- Overview
- Types of Breast Reconstruction
- Past Controversy over Silicone-Filled Breast Implants
- Finding a Plastic Surgeon
- Possible Complications With Breast Reconstruction
- Advantages and Disadvantages to Immediate Breast Reconstruction
- Health Insurance Coverage for Breast Reconstruction
- Breast Imaging After Reconstruction
- Additional Resources and References
 |
| Post-mastectomy
scar. Image Courtesy of Allergan, Inc. |
Breast reconstruction is a surgical procedure to rebuild the contour of the breast, along with the nipple and areola (the pigmented area surrounding the nipple) if desired. Recent advances in reconstructive techniques have given patients more choices when it comes to breast reconstruction, including the option to have breast reconstruction during the same operation in which the breast is removed. While a breast cancer diagnosis requires timely treatment decisions, most women have a sufficient amount of time to research treatment and reconstructive options before breast cancer surgery.
Though some women are not interested in breast reconstruction, many breast specialists support reconstructive surgery as an important option for patients to consider. Women are encouraged to weigh both the advantages and disadvantages of breast reconstruction with their plastic surgeons and cancer treatment team and make an informed decision based on their own situation. Breast reconstruction is most often an option for women who have had mastectomy if their entire breast has been removed. Women who undergo lumpectomy (surgical removal of a breast lump and a margin of surrounding tissue) rarely need breast reconstruction.
The goal of breast reconstruction is to create breast symmetry when a woman is wearing a bra. When a woman is nude, the reconstructed breast will look different from the unaffected breast, regardless of the type of reconstruction chosen. However, when a woman is wearing a bra, the size and shape of the reconstructed breast should closely resemble the unaffected breast.
It is a common misconception that women may have to wait a year or longer to begin the reconstructive progress after breast surgery. Though breast cancer patients who receive chemotherapy after mastectomy may have to delay reconstruction under chemotherapy is finished, the majority of women begin may reconstruction soon after the surgery in which the breast is removed (if not during the same operation).
There are two main types of breast reconstruction available to most mastectomy patients:
- Breast implants
- Muscle flap reconstruction
 |
| Breast reconstruction
with implant. Image courtesy of Allergan, Inc. |
The insertion of breast implants is usually a two-part procedure. The first implant operation involves placing a tissue expander in the intended breast area beneath the skin and chest muscle. The tissue expander is similar to a balloon, and the surgeon will fill the expander with salt-water solution periodically (usually once a week). The procedure to insert the tissue expander into the breast area typically takes about forty-five minutes. After the skin has sufficiently stretched, the surgeon will replace the tissue expander with a permanent implant, usually three to four months after the first implant surgery. Occasionally, a woman will not need a tissue expander. If this is the case, then the surgeon will proceed directly to permanent implant surgery. Approximately 50% of implants need some type of modification or replacement after five or ten years.
Muscle flap procedures take much longer than implant operations, lasting about four to five hours, and patients typically stay in the hospital three to four days, compared to one day with the implant operation. Though the recovery is slower, the breast usually looks and feels more natural to most women.
Because muscle flap reconstruction involves the blood vessels, women who smoke or have diabetes, vascular, or connective tissue diseases cannot typically undergo this type of breast reconstruction.
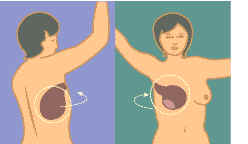 |
Latissimus dorsi muscle flap (back tissue) reconstruction. Image courtesy of NIH/NCI. |
Because many breast cancers involve the nipple areolar complex, the surgeon usually removes the nipple during mastectomy. After the breast volume has been rebuilt with a tissue expander or muscle flap procedure, the nipple may be recreated. Most nipple recreation takes place two to six months after the initial breast reconstruction to allow the new breast area ample time to heal. A new nipple may be created from a skin graft from a woman’s inner thigh or from the areola (the pigmented region surrounding the nipple) on her natural breast. Occasionally after a skin graft, the skin of the newly created nipple turns white. Some surgeons prefer to tattoo the skin graft of the new nipple to ensure that the color matches the color of the nipple from the natural breast.
To learn about advances in breast reconstruction, please visit http://www.imaginis.com/breasthealth/advances_breast_reconstruction.asp
Both saline and silicone-filled breast implants are reconstructive options for many breast cancer patients. However, many women will recall past controversy about silicone-filled implants. In 1992, the U.S. Food and Drug Administration imposed a ban on the general use of silicone gel-filled breast implants. Silicone implants were only allowed in closely monitored medical trials until they are determined to be safe for widespread use. Questions concerning the safety of silicone implants arose after manufacturing defects and implant misuse led to silicone leakage and rupturing in many patients. When silicone gel is free in breast tissue, it was thought that it could move to nearby tissues or to the lymph nodes. Some physicians attributed silicone leakage to immune-related disorders and other sicknesses. Many women who experienced silicone leakage reported:
-
breast pain
fatigue
myalgias (muscle pain)
arthralgias (joint pain)
hair loss
memory loss
After extensive study of the safety of silicone-filled breast implants, the FDA ruled that certain silicone-filled breast implants may be used during breast augmentation and reconstructive surgeries. Those implants must be made by Allergan or Mentor and can only be used for augmentation in women 22 years of age or older and for reconstruction in women of any age. By contrast, the FDA has approved saline-filled implants made by either Allergan or Mentor for breast augmentation in women aged 18 or older and for reconstruction in women of any age. The reason for the difference in age requirements is, according to the FDA, due to differences in risks among the implants. For example, silicone gel-filled implants will require frequent MRI monitoring to detect silent rupture (a rupture that can go undetected by the patient or physician). There is no risk of silent rupture for saline-filled implants. In addition, the health consequences of a ruptured saline-filled breast implant are different from those of a ruptured silicone gel-filled breast implant (see section below on Possible Complications With Breast Reconstruction for more information). Any implant other than the four named above is considered by the FDA to be "investigative" and women must be part of clinical trial in order to receive it.
If a woman is contemplating breast reconstruction, she should discuss her options with a plastic surgeon. It is important to make sure that the plastic surgeon is certified by the American Society of Plastic Surgeons and has experience with breast reconstruction.
Women may contact the American Society of Plastic Surgeons (ASPS) at 1-800-635-0635 to find out if their plastic surgeon is board certified. The ASPS was formed in 1972 and provides women with a list of ASPS certified members in the caller’s area. The ASPS website also allows women to search for a plastic surgeon by name, city, state, or zip code.
| The most common side effect of saline implants is capsular contracture-the scar around the implant begins to tighten and squeezes down on the soft implant, causing the breast to feel hard. |
As with any type of surgery, breast reconstruction has certain risks women should consider before deciding on reconstructive surgery. The most common complication with breast implants is capsular contracture: the scar or capsule around the implant begins to tighten and squeezes down on the soft implant, causing the breast to feel hard. Capsular contracture may be treated with additional surgery to remove the scar tissue. Occasionally, patients with capsular contracture may have to have the breast implant removed and replaced with a new one.
Another risk associated with breast implants is the possibility of rupture. If a saline-filled breast implant ruptures, the patient and physician will know because the implant will deflate and the saline solution leaks into the body immediately or over a period of days. The implant will lose its original size or shape. On the other hand, silicone-filled implant ruptures are called silent rupture because the patient and physician must not know that a rupture has occurred. Thus, the FDA recommends that patients with silicone-filled implants received an MRI three years after implantation and then every two years thereafter to screen for a rupture. However, some patients will experience symptoms of a rupture, including hard knots or lumps surrounding the implant or in the armpit, change or loss of size or shape of the breast or implant, pain, tingling, swelling, numbness, burning, or hardening of the breast.
Health experts do not know all of the reasons that breast implants might rupture. However, according to the FDA, some of the causes include:
- damage during implantation or during other surgical procedures
- folding or wrinkling of the implant shell
- trauma or other excessive force to the chest
- compression of the breast during mammography
Other rare complications from general surgery may also occur during breast reconstruction, including: bleeding, fluid collection, excessive scar tissue, infection, and problems with anesthesia. Women who smoke may experience a slower rate of healing or more noticeable scars since nicotine often interferes with the body’s natural healing process. Rarely, these complications may require additional surgery.
Note: It is not possible for women to breast-feed from the reconstructed breast. Even with nipple reconstruction and tattooing of the areola, the breast still lacks the proper glandular tissue and ducts necessary to produce milk. There has been no evidence that breast reconstruction causes a recurrence of breast cancer.
The majority of women diagnosed with breast cancer will undergo some type of breast surgery as part of their treatment. For many simple or modified radical mastectomy patients, breast reconstruction may be possible during the same surgical procedure (this is called immediate breast reconstruction). However, there are advantages and disadvantages to immediate breast reconstruction:
Advantages to immediate breast reconstruction:
- Patients do not wake up to the "shock" of losing a breast.
- Patients may avoid additional reconstructive surgery.
- Many doctors agree that the best-looking results occur when the cancer surgeon and the plastic surgeon plan the operation together.
Disadvantages to immediate breast reconstruction:
- Patients may find it emotionally difficult to weigh all of their breast reconstruction options while also dealing with their recent breast cancer diagnosis and treatment alternatives.
- If surgeons find that the cancer is more advanced than they initially thought, breast reconstruction may interfere with treatment (such as chemotherapy or radiation therapy).
Some doctors recommend that women who need radiation therapy after breast surgery have delayed breast reconstruction. Though radiation after the insertion saline implants or muscle flap procedures may potentially distort the breasts, this is rare. Radiation therapy can usually be administered to patients after breast reconstruction without any significant consequences.
Usually women who have breast reconstruction may choose to have the nipple and areola (the pigmented region surrounding the nipple) reconstructed during additional surgeries. Nipple and areola reconstruction occurs after the breast has had time to settle after the initial reconstructive surgery. Tissue for the nipple can be taken from the newly created breast, the opposite nipple, or even the ear. Tissue for the areola can be taken from the upper inner thigh. To match the other nipple and to create the areola, tattooing may be done.
The American Cancer Society suggests breast cancer patients ask their plastic surgeons the following questions before having breast reconstructive surgery:
- Am I a candidate for breast reconstruction?
- When can I have reconstruction?
- What types of reconstruction are possible for me?
- What is the average cost of each type of reconstruction and does insurance typically cover them?
- What type of reconstruction is best for me? Why?
- How much experience do you (plastic surgeon) have with this
- procedure?
- What results are realistic for me?
- Will the reconstructed breast match my remaining breast in
- size?
- How will my reconstructed breast feel to the touch?
- Will I have any feeling in my reconstructed breast?
- What possible complications should I know about?
- How much discomfort will I feel?
- How long will I be in the hospital?
- Will I need blood transfusions?
- If so, can I donate my own blood?
- How long is the recovery time?
- When can I begin to exercise? Play sports?
- Are there any patients I can speak with who have had the same surgery?
- Will reconstruction interfere with chemotherapy?
- Will reconstruction interfere with radiation therapy?
- How long will the implant last?
- What kind of changes to the breast can I expect over time?
- How will aging affect the reconstructed breast?
- What happens if I gain or lose weight?
- What new reconstruction options should I know about?(1)
Most health insurance companies do cover the cost of breast reconstruction after mastectomy. According to the American Society of Plastic and Reconstructive Surgeons, the average surgeon fee for breast reconstruction is $3618 for breast implant surgery not including bills from anesthesiologists, hospitals, or the cost of implants. In 1998, the Women's Health and Cancer Rights Act was passed, which requires all health insurance providers who cover mastectomy procedure to also cover the costs of breast cancer reconstruction for mastectomy patients. Under this legislation, insurance companies who cover the cost of mastectomy must also cover the costs of the following:
- reconstruction on the post-mastectomy breast
- surgery and reconstruction on the other breast to create symmetry
- breast prostheses
- treatment of complications from mastectomy, including lymphedema (chronic swelling) of the arm
It is important for women who have had breast reconstruction to continue receiving yearly mammography on the normal breast. Women who have had breast reconstruction should also practice monthly breast self-examination (BSE) and have yearly clinical breast exam. Click here to learn more about the guidelines for early detection of breast cancer.
Many radiologists do not take screening images of the area where the breast was removed (even if an implant or tissue flap is present) unless there is a clinical concern (for example, a new lump is found). Imaging breasts with implants requires a radiologist to take several special mammography views so he or she may see both the breast tissue and the implant. For this reason, diagnostic mammography is usually performed on women after breast reconstruction. Diagnostic mammography involves pinpointing the exact size and location of breast abnormalities as well as imaging the surrounding breast tissue and lymph nodes. Click here to learn more about mammography with breast implants.
In addition, women who receive silicone-filled breast implants are recommended to have MRI breast screening three years after implantation and every two years thereafter to screen for possible silent rupture.
- The American Cancer Society provides information on all aspects of breast reconstruction at http://www.cancer.org/.
- American Society of Plastic Surgeons provides information on breast reconstructive options at http://www.plasticsurgery.org/
- To learn about advances in breast reconstruction, please visit http://www.imaginis.com/breasthealth/advances_breast_reconstruction.asp
Updated: July 28, 2008



