- Who is a Candidate for Nuclear Medicine Breast Imaging?
- How is Nuclear Medicine Breast Imaging Performed?
- Recent Research on Nuclear Medicine Breast Imaging
Nuclear medicine breast imaging (also called scintimammography) is a supplemental breast exam that may be used in some patients to investigate a breast abnormality. A nuclear medicine test is not a primary investigative tool for breast cancer but can be helpful in selected cases after diagnostic mammography has been performed. Nuclear medicine breast imaging involves injecting a radioactive tracer (dye) into the patient. Since the dye accumulates differently in cancerous and non-cancerous tissues, scintimammography can help physicians determine whether cancer is present.
Currently, only the Miraluma Tc-99m sestamibi compound, manufactured by DuPont Pharmaceuticals, is approved by the Food and Drug Administration (FDA) for breast imaging in the United States. Therefore, the nuclear medicine breast imaging test may be referred to as a "Miraluma." Nuclear medicine may be appropriate in patients who have dense breast tissue that makes their mammograms difficult to interpret or in patients with palpable abnormalities (i.e., those able to be physically felt) but whose mammograms do not reveal any abnormalities.
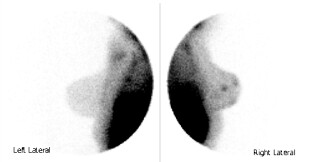 |
Nuclear medicine breast image, courtesy of Siemens Medical. |
Nuclear medicine breast imaging is not a screening tool for breast cancer. However, after a physical breast exam, mammography, and ultrasound are performed, nuclear medicine breast imaging may be appropriate for certain patients. Supplemental breast imaging helps determine whether a patient has a suspicious breast abnormality that would require a biopsy to confirm the presence of breast cancer.
Nuclear medicine breast imaging may be appropriate for patients with:
- Dense breast tissue
- Large, palpable (able to be felt) abnormalities that cannot be imaged well with mammography or ultrasound
- Breast implants
- When multiple tumors are suspected (see below)
- A lump at the surgical site after mastectomy (breast removal) since scar tissue may be difficult to distinguish from other tumors with other breast imaging exams
- To check the axillary (underarm) lymph nodes to determine whether they contain cancer cells (sentinel lymph node biopsy)
Like magnetic resonance imaging (MRI) of the breast, nuclear medicine may also be helpful to determine if multiple breast tumors are present. For instance, a mammogram or ultrasound (sonogram) of the breast may reveal breast cancer in one area. However, a nuclear medicine breast imaging test may show that the cancer is in fact multi-focal; tumors are present in several areas of the breast. Determining the extent of breast cancer with nuclear medicine can help indicate treatment: breast conserving surgery (lumpectomy) or breast removal (mastectomy). Mastectomy is indicated if there are multiple tumors.
Studies show that nuclear medicine breast imaging is only 40% to 60% accurate in imaging small breast abnormalities but more than 90% accurate in detecting abnormalities over one centimeter. However, mammography and physical exams are often very useful for detecting large abnormalities. It is the small abnormalities that tend to need additional imaging. Therefore, in this respect, nuclear medicine breast imaging is often of limited value.
 |
This image shows a patient prepared for a nuclear medicine breast imaging exam. |
The nuclear medicine breast imaging test takes approximately 45 minutes to one hour to perform and costs approximately $200 to $600 per exam. Nuclear medicine involves the use of radiation, but the dose is very low and is not harmful to patients. Most of the drug leaves the body within a few hours of the test.
To perform the exam, a radioactive tracer (Tc-99m sestamibi) is injected in the patient’s arm opposite of the breast being studied. Patients may experience a brief metallic taste after the tracer is injected. The radioactive tracer travels throughout the body, including to the breast that needs to be imaged. Normal tissue will only accumulate a small amount of the radioactive tracer (dye). However, cancer cells tend to take up more of the dye.
After the radioactive tracer has been injected, the patient is instructed to lie face down on a special table while the breast hangs down through a hole in the table. Approximately five minutes after the injection, a special gamma camera is used to capture images of the breast from several angles. This takes several minutes for each image that is taken. During this time, the patient should try to lie as still as possible. After all of the images are taken while the patient is lying face down on the table, she may be asked to sit up or raise her arms while additional images of her breast are taken. Unlike mammography, no breast compression is necessary during a nuclear medicine test (although mammography is performed prior to the recommendation of a nuclear medicine breast imaging test).



